Slowing dangerous bacteria may be more effective than killing them
Researchers at the University of Illinois have discovered a mechanism that allows bacteria of the same species to communicate when their survival is threatened. The study suggests that it may be possible to slow dangerous infections by manipulating the messages these microbes send to each other, allowing the body to defeat an infection without causing the bacteria to develop resistance to the treatment.
The study, reported in the Proceedings of the National Academy of Sciences, builds on work conducted by other researchers at Illinois, including biochemist John Woodland Hastings, who died in 2014, and John Cronan, a professor and the head of the department of microbiology.
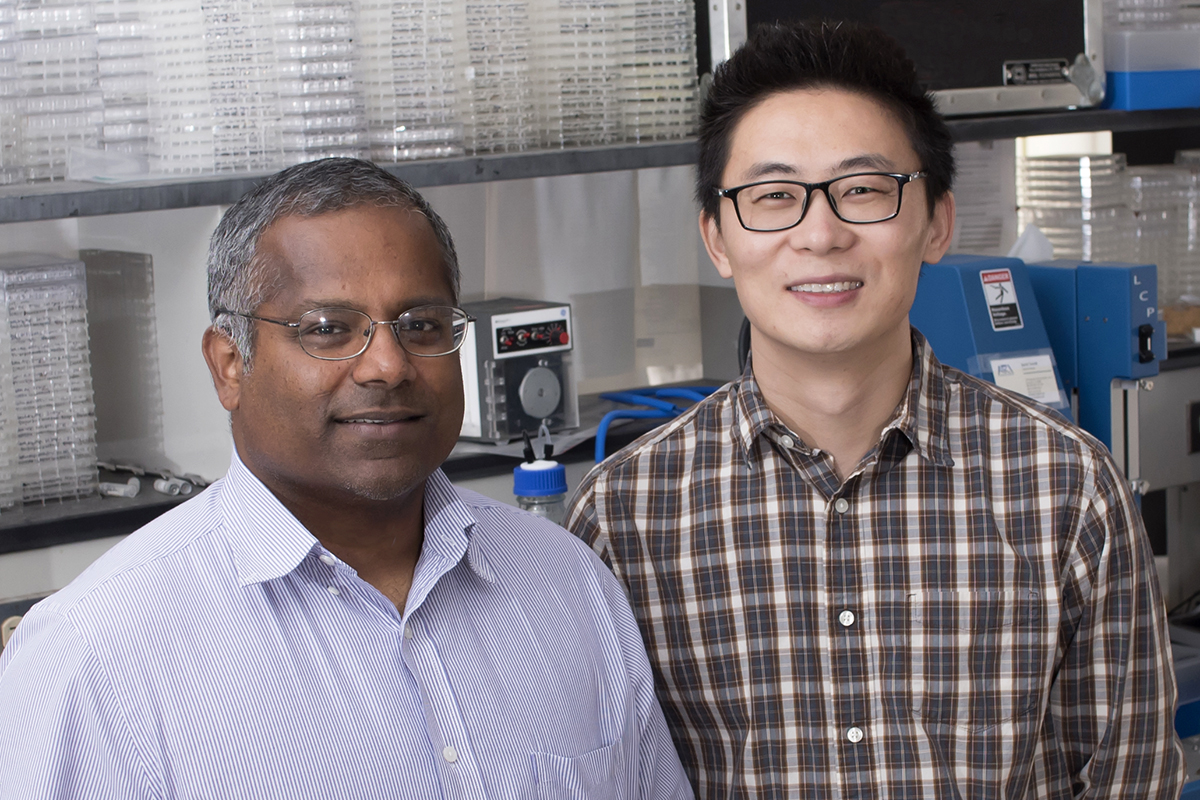
“Bacteria are intelligent little organisms. They can survive almost anywhere and quickly adapt to new conditions,” said U. of I. biochemistry professor Satish Nair, a co-author of the study with postdoctoral researcher Shi-Hui Dong and other colleagues. Nair is the director of the Center for Biophysics and Quantitative Biology at Illinois.
When bacteria compete with other microbes for scarce resources, the more successful group will produce a unique molecule – an antibiotic – to kill off the other species. When population growth of one group of bacteria outpaces availability of the nutrients it needs to survive, the group produces another unique molecule that tells it to go into a dormant, but more virulent, state and slow growth until more food is available, Nair said.
“Ever since Alexander Fleming discovered penicillin in 1928, we have been using antibiotic molecules developed by one microorganism to kill another microorganism,” Nair said. “Unfortunately, the bacteria have quickly adapted to resist antibiotics, and in a short time, antibiotics will be ineffective.
“On average, nearly every species of bacteria is resistant to at least one antibiotic. Two years ago, researchers in Europe and Asia discovered a so-called superbug that is resistant to all known antibiotics,” Nair said. “Bacteria can share adaptations very easily, and there are so many bacteria with different adaptations to share, which is why they can develop resistance so quickly.”
“Broad-spectrum antibiotics and the overuse of antibiotics are problematic because antibiotics kill off many types of bacteria, even good ones, and the survivors figure out ways to adapt, sharing their strategies with other bacteria,” Dong said.
“No pharmaceutical company is going to invest in 10 years’ worth of research and development if a new antibiotic has a shelf-life of only two years,” Nair said. “It’s not enough time to recover the costs of production.”

Nair and Dong’s new study targets the language, or group signal, that bacteria use to slow down growth rather than the antibiotic signal to kill. The researchers say understanding how bacteria produce the dormancy-signal molecule paves the way for developing molecules that can disrupt the communication of specific bacteria, with little chance for drug resistance to develop.
“We don’t need to kill bacteria to treat disease and infection; we can just slow them down and make them less potent,” Nair said. “That way, there is little chance for any resistance to develop.”
Nair is an IGB faculty member in the Mining Microbial Genomes and Microbiome Metabolic Engineering research themes. Research in the Nair lab is funded by the National Institutes of Health.
